Science, Art, Litt, Science based Art & Science Communication
Stop! You cannot go beyond this sign if you are not a trained scientist or a lab technician! Turn back and move away!
Ordinary people cannot enter a microbiology lab either in a research institution or in a hospital. Outside people like sci-artists who insist that they be allowed and work there without taking precautions will be turned down.
Why? Because there might be harmful agents that can cause diseases in both animals and human beings in these labs and if precautions are not taken, they might spread to the outside world. Scientists working in these labs must ensure that public outside be protected from the extremely dangerous agents they are working with. So they take several precautions and follow laborious biosafety procedures in order to do that.
But biosafety levels differ from country to country and in some parts of the world to your mental discomfort least precautions are taken while dealing with harmful agents for various reasons. Therefore, it is important to learn about biosafety.
A very specialized research laboratory that deals with infectious agents is the biosafety lab. Whether performing research or conducting probing tests or production activities (like developing vaccines), when working with infectious materials, organisms or perhaps even laboratory animals, the proper degree of protection is of utmost importance.
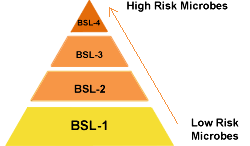
Protection for laboratory personnel, the environment and the local community must be considered and ensured. The protections required by these types of activities are defined as biosafety levels. Biological safety levels are ranked from one to four in most developed countries and are selected based on the agents or organisms on which the research or work is being conducted. Each level up builds on the previous level, adding constraints and barriers.
The four biosafety levels were developed to protect against a world of select agents. These agents include bacteria, fungi, parasites, prions, rickettsial agents and viruses, the last one being probably the largest and most important group. In many instances the work or research involves vertebrate animals, everything from mice to cattle to monkeys. When vertebrates are involved, additional precautions and safety requirements are necessary. Using the most infectious agents also means extensive security measures are in place, not only because of their virulence but also because of their potential for use in bioterrorism.
Picture credit: www.cdc.gov
Biosafety Level 1 Lab
Biosafety level one, the lowest level, applies to work with agents that usually pose a minimal potential threat to laboratory workers and the environment and do not consistently cause disease in healthy adults. Research with these agents is generally performed on standard open laboratory benches without the use of special containment equipment. BSL 1 labs are not usually isolated from the general building. Special containment equipment or facility design is not required, but may be used as determined by appropriate risk assessment. Training on the specific procedures is given to the lab personnel, who are supervised by a trained microbiologist or scientist.
Standard microbiology practices are usually enough to protect laboratory workers and other employees in the building. These include mechanical pipetting only (no mouth pipetting allowed). Persons must wash their hands after working with potentially hazardous materials and before leaving the laboratory. Eating, drinking, smoking, handling contact lenses, applying cosmetics, and storing food for human consumption must not be permitted in laboratory areas. Food must be stored outside the laboratory area in cabinets or refrigerators designated and used for this purpose. Safe cutting and piercing material (like knives, scalpels, needles) handling is a must. Used disposable needles and syringes must be carefully placed in conveniently located puncture-resistant containers used for sharps disposal. Non-disposable sharps must be placed in a hard walled container for transport to a processing area for decontamination, preferably by autoclaving. Broken glassware must not be handled directly. Instead, it must be removed using a brush and dustpan, tongs, or forceps. Plastic ware should be substituted for glassware whenever possible.
All procedures must be performed to minimize the creation of splashes or aerosols. Decontamination of all work surfaces when work is complete, e.g., daily. Decontamination of spills is done immediately, and all potentially infectious materials are decontaminated prior to disposal, generally by autoclaving (Autoclave is a term used mainly in laboratories whilst 'Sterilizer' is used more commonly for medical and pharmaceutical applications. An effective Autoclave or Sterilizer must contain dry saturated steam like in a cooker in a kitchen). Standard microbiological practices also require attention to personal hygiene. Normal laboratory personal protective equipment is generally worn, consisting of eye protection, gloves and a lab coat or gown. An effective integrated pest management program is required. The laboratory supervisor must ensure that laboratory personnel receive appropriate training regarding their duties, the necessary precautions to prevent exposures, and exposure evaluation procedures.
Laboratories should have doors for access control. Laboratories windows that open to the exterior should be fitted with screens. Biohazard signs are posted and access to the lab is limited whenever infectious agents are present.
Biosafety Level 2 Lab
Biosafety level two would cover work with agents associated with human disease, in other words, pathogenic or infectious organisms posing a moderate hazard. Examples are the equine encephalitis viruses and HIV when performing routine diagnostic procedures or work with clinical specimens. Therefore, because of their potential to cause human disease, great care is used to prevent percutaneous injury (needlesticks, cuts and other breaches of the skin), ingestion and mucous membrane exposures in addition to the standard microbiological practices of BSL 1. Contaminated sharp equipment is handled with extreme caution. Use of disposable syringe-needle units and appropriate puncture-resistant sharps containers is mandatory. Direct handling of broken glassware is prohibited, and decontamination of all sharp objects prior to disposal is standard practice. The laboratory’s written biosafety manual details any needed immunizations (e.g., hepatitis B vaccine or TB skin testing) and whether serum banking is required for at-risk lab personnel. Access to the lab is more controlled than for BSL 1 facilities. Immunocompromised, immunosuppressed and other persons with increased risk for infection may be denied admittance at the discretion of the laboratory director.
BSL 2 labs must also provide the next level of barriers, i.e., specialty safety equipment and facilities. Preferably, this is a Class II biosafety cabinet or equivalent containment device for work with agents and an autoclave or other suitable method for decontamination within the lab. A readily available eyewash station is needed. Selfclosing lockable doors and biohazard warning signs are also required at all access points.
laboratory personnel have specific training in handling pathogenic agents and are supervised by scientists competent in handling infectious agents and associated procedures; access to the laboratory is totally restricted when work is being conducted; and all procedures in which infectious aerosols or splashes may be created are conducted in BSCs or other physical containment equipment.
All persons entering the laboratory must be advised of the potential hazards and meet specific entry/exit requirements. Laboratory personnel must be provided medical surveillance, as appropriate, and offered available immunizations for agents handled or potentially present in the laboratory. A laboratory-specific biosafety manual must be prepared and adopted as policy. The biosafety manual must be available and accessible to all the people working in the lab.
Potentially infectious materials must be placed in a durable, leak proof container during collection, handling, processing, storage, or transport within a facility. Laboratory equipment should be routinely decontaminated, as well as, after spills, splashes, or other potential contamination. Equipment must be decontaminated before repair, maintenance, or removal from the laboratory.
Incidents that may result in exposure to infectious materials must be immediately evaluated and treated according to procedures described in the laboratory biosafety manual. All such incidents must be reported to the laboratory supervisor. Medical evaluation, surveillance, and treatment should be provided and appropriate records maintained. Animal and plants not associated with the work being performed must not be permitted in the laboratory.
Only authorized persons will be allowed into these level 2,3 and 4 labs.
Biosafety Level 3 Lab
Biosafety Level 3 is applicable to clinical, diagnostic, teaching, research, or production facilities where work is performed with indigenous or exotic agents that may cause serious or potentially lethal disease through the inhalation route of exposure. Laboratory personnel must receive specific training in handling pathogenic and potentially lethal agents, and must be supervised by scientists competent in handling infectious agents and associated procedures. All procedures involving the manipulation of infectious materials must be conducted within BSCs (Biosafety cabinets used in research labs) or other physical containment devices.
Yellow fever, encephalitis and West Nile virus are examples of agents requiring biosafety level 3 practices and containment. Work with these agents is strictly controlled and must be registered with all appropriate government agencies. These are indigenous or exotic agents that may cause serious or lethal disease via aerosol transmission, i.e., simple inhalation of particles or droplets. The pathogenicity and communicability of these agents dictates the next level of protective procedures and barriers. Add to all the BSL 2 practices and equipment even more stringent access control and decontamination of all wastes, including lab clothing before laundering, within the lab facility. Baseline serum samples are collected from all lab and other at-risk personnel as appropriate.
Laboratory personnel must be provided medical surveillance and offered appropriate immunizations for agents handled or potentially present in the laboratory.
More protective primary barriers are used in BSL 3 laboratories, including solid-front wraparound gowns, scrub suits or coveralls made of standard materials and respirators as necessary. Facility design should incorporate self-closing double-door access separated from general building corridors.
A BSL-3 laboratory has special engineering and design features.
Laboratory doors must have locks in accordance with the institutional policies. The laboratory must be separated from areas that are open to unrestricted traffic flow within the building. Laboratory access is restricted. Access to the laboratory is through two self-closing doors. A clothing change room (anteroom) may be included in the passageway between the two self-closing doors.
Floors must be slip resistant, impervious to liquids, and resistant to chemicals. Consideration should be given to the installation of seamless, sealed, resilient or poured floors, with integral cove bases. Walls should be constructed to produce a sealed smooth finish that can be easily cleaned and decontaminated. Ceilings should be constructed, sealed, and finished in the same general manner as walls.
The ventilation must provide ducted, directional airflow by drawing air into the lab from clean areas and with no recirculation. All windows in the laboratory must be sealed.
Laboratory personnel must be able to verify directional airflow. A visual monitoring device, which confirms directional airflow, must be provided at the laboratory entry. Audible alarms should be considered to notify personnel of air flow disruption.
The laboratory exhaust air must not re-circulate to any other area of the building. The laboratory building exhaust air should be dispersed away from occupied areas and from building air intake locations or the exhaust air must be HEPA filtered (High-efficiency particulate arrestance, also sometimes called high-efficiency particulate arresting or high-efficiency particulate air, is a type of air filter). HEPA filter housings should have gas-tight isolation dampers, decontamination ports, and/or bag-in/bag-out (with appropriate decontamination procedures) capability. The HEPA filter housing should allow for leak testing of each filter and assembly. The filters and the housing should be certified at least annually. HEPA filtered exhaust air from a Class II BSC can be safely re-circulated into the laboratory environment if the cabinet is tested and certified at least annually and operated according to manufacturer’s recommendations.
Equipment that may produce infectious aerosols must be contained in primary barrier devices that exhaust air through HEPA filtration or other equivalent technology before being discharged into the laboratory. These HEPA filters should be tested and/or replaced at least annually.
Decontamination of the entire laboratory should be considered when there has been gross contamination of the space, significant changes in laboratory usage, for major renovations, or maintenance shut downs. Selection of the appropriate materials and methods used to decontaminate the laboratory must be based on the risk assessment.
Biosafety Level 4 Lab
Biosafety Level 4 is required for work with extremely dangerous and exotic agents that pose a high individual risk of aerosol-transmitted laboratory infections and life-threatening disease that is frequently fatal, for which there are no vaccines or treatments, or a related agent with unknown risk of transmission. Examples are the Ebola virus, the Lassa virus. These facilities provide the maximum protection and containment.
Agents with a close or identical antigenic relationship to agents requiring BSL-4 containment must be handled at this level until sufficient data are obtained either to confirm continued work at this level, or re-designate the level. Laboratory staff must have specific and thorough training in handling extremely hazardous infectious agents. Laboratory staff must understand the primary and secondary containment functions of standard and special practices, containment equipment, and laboratory design characteristics. All laboratory staff and supervisors must be competent in handling agents and procedures requiring BSL-4 containment. The laboratory supervisor in accordance with institutional policies controls access to the laboratory.
To the BSL 3 practices, more requirements are added for complete clothing change before entry, a shower on exit and decontamination of all materials prior to leaving the facility.
There are two models for BSL-4 laboratories: 1. A Cabinet Laboratory—Manipulation of agents must be performed in a Class III BSC; and 2. A Suit Laboratory—Personnel must wear a positive pressure supplied air protective suit. BSL-4 cabinet and suit laboratories have special engineering and design features to prevent microorganisms from being disseminated into the environment.
All persons entering the laboratory must be advised of the potential hazards and meet specific entry requirements in accordance with institutional policies. Only persons whose presence in the facility or individual laboratory rooms is required for scientific or support purposes are authorized to enter. Entry into the facility must be limited by means of secure, locked doors. A logbook, or other means of documenting the date and time of all persons entering and leaving the laboratory must be maintained.
While the laboratory is operational, personnel must enter and exit the laboratory through the clothing change and shower rooms except during emergencies. All personal clothing must be removed in the outer clothing change room. All persons entering the laboratory must use laboratory clothing, including undergarments, pants, shirts, jumpsuits, shoes, and gloves (as appropriate). All persons leaving the laboratory must take a personal body shower. Used laboratory clothing must not be removed from the inner change room through the personal shower. These items must be treated as contaminated materials and decontaminated before laundering. After the laboratory has been completely decontaminated and all infectious agents are secured, necessary staff may enter and exit without following the clothing change and shower requirements described above.
The BSL 4 laboratory should contain a Class III biological safety cabinet but may use a Class I or II BSC in combination with a positive-pressure, air-supplied full-body suit. Usually, BSL 4 laboratories are in separate buildings or a totally isolated zone with dedicated supply and exhaust ventilation. Exhaust streams are filtered through high-efficiency particulate air (HEPA) filters, depending on the agents used.
Only necessary equipment and supplies should be stored inside the BSL-4 laboratory. All equipment and supplies taken inside the laboratory must be decontaminated before removal from the laboratory. Daily inspections of essential containment and life support systems must be completed and documented before laboratory work is initiated to ensure that the laboratory is operating according to established parameters.
Practical and effective protocols for emergency situations must be established. These protocols must include plans for medical emergencies, facility malfunctions, fires, escape of animals within the laboratory, and other potential emergencies. Training in emergency response procedures must be provided to emergency response personnel and other responsible staff according to institutional policies.
All manipulations of infectious materials within the laboratory must be conducted in the Class III biological safety cabinet. Double-door, pass through autoclaves must be provided for decontaminating materials passing out of the Class III BSC(s). The autoclave doors must be interlocked so that only one can be opened at any time and be automatically controlled so that the outside door to the autoclave can only be opened after the decontamination cycle has been completed.
Workers in the laboratory must wear protective laboratory clothing with a solid-front, such as tie-back or wrap-around gowns, scrub suits, or coveralls. No personal clothing, jewelry, or other items except eyeglasses should be taken past the personal shower area. All protective clothing must be removed in the dirty side change room before showering. Reusable clothing must be autoclaved prior to removal from the laboratory for laundering. Eye, face and respiratory protection should be used in rooms containing infected animals as determined by the risk assessment. Prescription eyeglasses must be decontaminated before removal through the personal body shower.
Disposable gloves must be worn underneath cabinet gloves to protect the worker from exposure should a break or tear occur in a cabinet glove. Gloves must not be worn outside the laboratory. Alternatives to latex gloves should be available. One should not wash or reuse disposable gloves. Used gloves with other contaminated laboratory waste should be disposed as per rules immediately.
All procedures must be conducted by personnel wearing a one-piece positive pressure supplied air suit. Workers must wear laboratory clothing, such as scrub suits, before entering the room used for donning positive pressure suits. Decontamination of outer suit gloves is performed during laboratory operations to remove gross contamination and minimize further contamination of the laboratory.
The BSL-4 cabinet laboratory consists of either a separate building or a clearly demarcated and isolated zone within a building. Laboratory doors must have locks in accordance with the institutional policies.
Rooms in the facility must be arranged to ensure sequential passage through an inner (dirty) changing area, a personal shower and an outer (clean) change room upon exiting the room(s) containing the Class III BSC(s).
An automatically activated emergency power source must be provided at a minimum for the laboratory exhaust system, life support systems, alarms, lighting, entry and exit controls, BSCs, and door gaskets. Monitoring and control systems for air supply, exhaust, life support, alarms, entry and exit controls, and security systems should be on an uninterrupted power supply (UPS). A double-door autoclave, dunk tank, fumigation chamber, or ventilated airlock must be provided at the containment barrier for the passage of materials, supplies, or equipment.
A hands-free sink must be provided near the door of the cabinet room(s) and the inner change room. A sink must be provided in the outer change room. All sinks in the room(s) containing the Class III BSC must be connected to the wastewater decontamination system.
Drains in the laboratory floor (if present) must be connected directly to the liquid waste decontamination system. Services and plumbing that penetrate the laboratory walls, floors, or ceiling must be installed to ensure that no backflow from the laboratory occurs. These penetrations must be fitted with two (in series) backflow prevention devices. Consideration should be given to locating these devices outside of containment. Atmospheric venting systems must be provided with two HEPA filters in series and be sealed up to the second filter. Decontamination of the entire cabinet must be performed using a validated gaseous or vapor method when there have been significant changes in cabinet usage, before major renovations or maintenance shut downs, and in other situations, as determined by risk assessment.
Entry into the BSL-4 laboratory must be through an airlock fitted with airtight doors. Personnel who enter this area must wear a positive pressure suit supplied with HEPA filtered breathing air. The breathing air systems must have redundant compressors, failure alarms and emergency backup. A chemical shower must be provided to decontaminate the surface of the positive pressure suit before the worker leaves the laboratory. In the event of an emergency exit or failure of the chemical shower system, a method for decontaminating positive pressure suits, such as a gravity fed supply of chemical disinfectant, is needed. An automatically activated emergency power source must be provided, at a minimum, for the laboratory exhaust system, life support systems, alarms, lighting, entry and exit controls, BSCs, and door gaskets. Doors and windows should be break resistant.
Liquid effluents from chemical showers, sinks, floor drains, autoclave chambers, and other sources within the laboratory must be decontaminated by a proven method, preferably heat treatment, before being discharged to the sanitary sewer.
We have touched on only the main issues and differences between BSL 1, 2, 3 and 4 laboratories. There are many other concerns and requirements addressed in the CDC and medical council, research and lab manuals, such as impervious, easy-to-clean surfaces; insect and rodent control; and total barrier sealing of all wall, floor and ceiling penetrations. Our aim is just to give a brief introduction but people working in these labs follow very strict and detailed procedures to protect people outside as public safety is the utmost importance to the scientists working in the field.
Biosafety Level 4 from State of Tomorrow on Vimeo.
Source: Biosafety
Views: 1182
Replies to This Discussion
-
1041
Why scientists are concerned about leaks at biolabs
https://medicalxpress.com/news/2021-05-scientists-leaks-biolabs.htm...
-
-
How do coronavirus researchers avoid catching COVID-19?
Around the world, virologists in labs are constantly handling samples of SARS-CoV-2, the virus that causes COVID-19, as part of our global quest to understand, and hopefully overcome, this pandemic. We know that SARS-CoV-2 is highly infectious and can be lethal if it gets inside our bodies. So it’s vital these scientists are protected from becoming infected.
This is nothing new. Virologists regularly handle large quantities of virus in much more concentrated forms than we would encounter in the outside world. So how do we stay safe from these pathogens?
There are a lot of different levels of protection we use, but what it all comes down to is trust and responsibility.
Procedure and protocols
Before anyone gets near new viruses in the lab, we need permission from the relevant government authority. We inform them of what we intend to do with the virus and demonstrate we can work with it in a safe and secure environment.
When it comes to working with the virus in the lab, we have carefully written documents detailing how to handle the pathogens so that everyone stays safe. This includes using specialist screw-top lids to store virus samples to prevent spills, and treating all liquids in the facility as infectious – even if it’s a newly opened bottle of sterile water.
Scientists who work on hazardous viruses have also undergone significant training. This includes academic qualifications and laboratory experience, but also specific instruction in handling pathogens safely. Each user must have a minimum number of hours of training, covering all procedures used in the facility, and eventually signed off by an experienced virologist and biosafety officer.
Equipment
A lot of the physical protection from the viruses we work on comes from the environment in which they are handled. We have separate rooms for virus work and non-virus work to prevent contamination.
Hazardous viruses are handled in specialist cabinets that have controlled sterile airflow. This protects the user from the pathogens as air is restricted from leaving the cabinet, and protects samples inside the cabinet from the user. There are many microbes in the air and on our skin, and we don’t want our experimental samples getting contaminated with any of these.
Read more: My new life as a coronavirus tester – a scientist's story
In higher containment facilities, like those used for SARS-CoV-2, the entire room is maintained under negative pressure – the air pressure inside the lab is lower than the air pressure outside it. No air can leave these rooms without going through a specialist filter that removes potential pathogens.
Cleaning
A large amount of virology revolves around cleaning up. Cabinets are cleaned with alcohol before and after use, as is anything taken in or out of them. In addition to cleaning surfaces, anything used inside virus labs must be disinfected before removal. All tubes, flasks and so on are chemically disinfected and then cleaned with an autoclave – an industrial sterilisation unit that uses high pressure and temperature to remove pathogens.
As an extra precaution in higher containment facilities, regular fumigation is performed where the entire room is sealed and pumped full of formaldehyde gas to neutralise any lingering pathogens.
Personal protective equipment
I’ve deliberately left personal protective equipment, or PPE, quite low down this list. That’s because PPE is considered the final barrier of protection. If protocols are followed and equipment used correctly, there should be no instances of a lab user being exposed to a virus sample. Unfortunately we cannot foresee all incidents and scientists are only human, so PPE is crucial to safe lab work. PPE also protects our samples from us. We have lots of microbes and enzymes on our skin that we don’t want in our experiments.
In labs handling mild risk pathogens, scientists wear lab coats and gloves (sometimes also eye protection where necessary). Pathogens are unlikely to leave the cabinet but if they do, they would only cause mild illness to healthy individuals so no more PPE is required.
Working in higher containment where pathogens are more likely to be transmitted or cause more serious illness (or both), significantly more PPE is used. Rules in these facilities vary as they are tailored specifically to the pathogens handled, but in general, full biohazard suits are worn which are sealed at the ankles and wrists. Specialist footwear is worn, gloves are doubled up (in case one layer of glove becomes compromised).
Inside the high-security lab at Queens University, Belfast. Grace C Roberts/QUB, Author provided (No reuse)
For viruses such as SARS-CoV-2 that infect the respiratory system, goggles and FFP3 masks which are specifically fitted to individual users are worn to protect from exposure via inhalation or through the eyes. All these items of PPE are worn so that, in the unlikely case of a spill, workers have time to exit the facility without exposing themselves to infection.
It all comes down to responsibility
No matter the pathogen, regulations, or set-up of a laboratory, our main form of protection from viruses is the scientists themselves. Everything discussed in this article is only effective if every scientist in the lab follows all the regulations and has the right training.
There is little point donning all your PPE if the person who used the lab before you did not follow procedure – for example, if there was an unreported spill or a used scalpel blade left out on the benchtop. It is up to all of us to keep ourselves, our colleagues, and the outer world safe.
This ethos is also relevant to our daily lives during the pandemic. It is important to notify the lab of spills in the lab, just as it is important that we report COVID-19 symptoms or a positive test result. It’s important that we leave our lab space clean and tidy for other uses, much like it is important to regularly wash our hands. It’s important we wear PPE in the lab to protect ourselves and our samples, much like we need to wear masks properly to protect those around us in public.
Finally, like in the lab where we treat any and all liquids used in the virus facility as infectious, in the outer world we must treat ourselves and those around us as potentially infectious at all times. If we want to beat this pandemic, we all need to think a little more like virologists.
https://theconversation.com/how-do-coronavirus-researchers-avoid-ca...
-
-
Essential features of a biosafety level 4 (BSL-4) laboratory
-
© 2025 Created by Dr. Krishna Kumari Challa.
Powered by
![]()