Science, Art, Litt, Science based Art & Science Communication
The epidemic of mucormycosis is yet another of the unpleasant surprises produced by the COVID pandemic—following MIS-C, a severe inflammatory syndrome that seems to mostly affect children, and “long COVID,” a complex of symptoms that continue to afflict patients months after initial infection. Mucormycosis is one of an array of ferocious fungal diseases that have attacked COVID patients, including a lethal yeast called Candida auris and a spate of infections with Aspergillus fungi that have earned the acronym CAPA (for COVID-associated pulmonary aspergillosis).
Mucormycosis, formerly known as zygomycosis, is the disease caused by the many fungi that belong to the fungal family “Mucorales”.
The member of this family which most often causes infection in humans is called Rhizopus oryzae. In India though, another family member called Apophysomyces, found in tropical and subtropical climates, is also common.
Some COVID-19 patients in India have developed a rare and potentially fatal fungal infection called mucormycosis, also known as "black fungus," according to reports.
Mucormycosis is caused by a group of molds called mucormycetes, which grow in soil and decaying organic matter, such as rotting leaves and wood. It is ubiquitous and found in soil, manure, decaying organic matter and air and even in the nose and mucus of healthy people.
In the lab, these fungi grow rapidly and have a black/brown fuzzy appearance.
The family members causing human disease grow well at body temperature and in an acidic environment (seen when tissue is dead or dying or with uncontrolled diabetes).
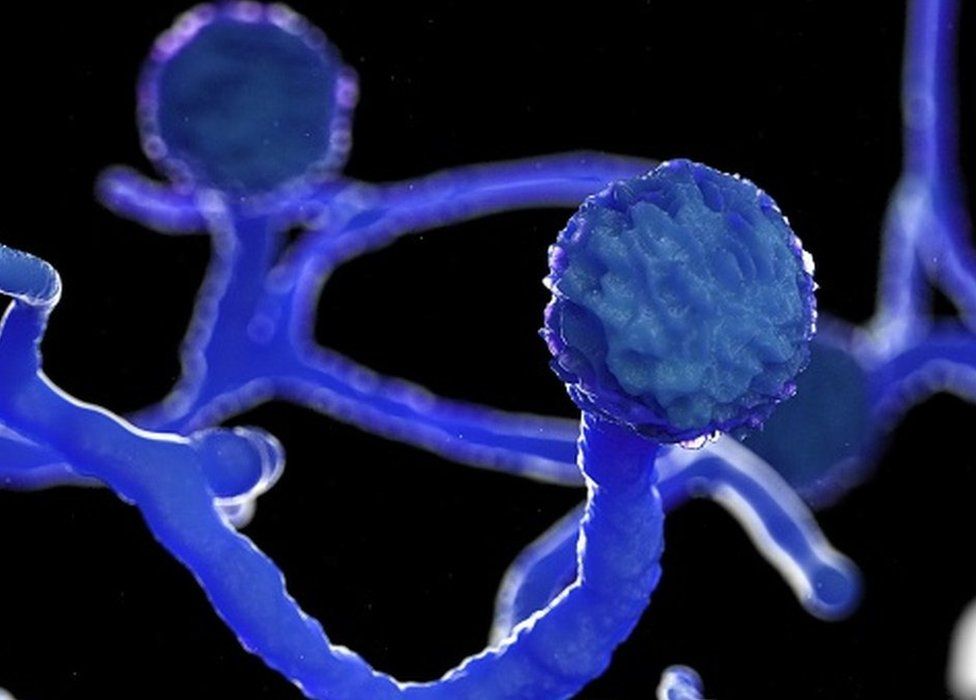 IMAGE Source: GETTY IMAGES
IMAGE Source: GETTY IMAGESMucorales are considered opportunistic fungi, meaning they usually infect people with an impaired immune system, or with damaged tissue.
The mold can enter the body through cuts and other abrasions in the skin, or the infection can take hold in the sinuses or lungs after people breathe in the fungal spores. Once inside the body, the fungus can sometimes spread through the bloodstream and affect other organs, such as the brain, eyes, nose, spleen and heart.
There are three ways humans can contract mucormycosis — by inhaling spores, by swallowing spores in food or medicines, or when spores contaminate wounds.
Inhalation is most common. We actually breathe in the spores of many fungi every day. But our immune system and healthy lungs generally prevent them from causing an infection.
When the lungs are damaged and the immune system is suppressed, such as is the case in patients with severe COVID, these spores can grow in our airways or sinuses and invade our bodies’ tissue.
Mucormycosis can manifest in the lungs, but the nose and sinuses are the most common site of mucormycosis infection. From there it can spread to the eyes, potentially causing blindness, or the brain, causing headache or seizures.
It can also affect the skin. Life-threatening wound infections have been seen after injuries sustained during natural disasters or on battle fields where wounds have been contaminated by soil and water.
Image source: Google images
Most commonly, mucormycosis strikes those with weakened immune systems, including those with diabetes and those taking medicines that suppress immune activity. Now, an increasing number of COVID-19 patients in India appear to be contracting the infection. It has an overall mortality rate of 50% if not treated. Some lose eyes and part of noses.
Patients suffering from the fungal infection typically have symptoms of stuffy and bleeding nose; swelling of and pain in the eye; drooping of eyelids; and blurred and finally, loss of vision. There could be black patches of skin around the nose.One can also experience loose tooth , tooth pain , ulcer over hard palate , facial pain , numbness eye pain , restricted eye mobility,eye swelling, blood discharge from nose ,nasal stuffiness , pain over malar region , decreased vision , sinus like symptoms.

Doctors say most of their patients arrive late, when they are already losing vision, and doctors have to surgically remove the eye to stop the infection from reaching the brain.
In some cases, doctors in India say, patients have lost their vision in both eyes. And in rare cases, doctors have to surgically remove the jaw bone in order to stop the disease from spreading.
An anti-fungal intravenous injection which costs 3,500 rupees ($48) a dose and has to be administered every day for up to eight weeks is the only drug effective against the disease.
Cases are appearing throughout India now.
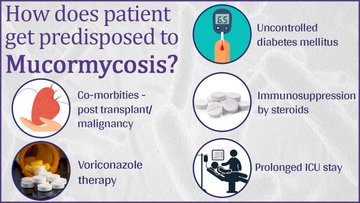
The rise in cases may be connected to the use of steroids in hospitalized COVID-19 patients, since the drugs suppress the immune system.
And those with diabetes start out at increased risk for the infection, even before taking steroids.
Steroids reduce inflammation in the lungs for Covid-19 and appear to help stop some of the damage that can happen when the body's immune system goes into overdrive to fight off coronavirus. But they also reduce immunity and push up blood sugar levels in both diabetics and non-diabetic Covid-19 patients.
It's thought that this drop in immunity could be triggering these cases of mucormycosis.
Diabetes lowers the body's immune defenses, coronavirus exacerbates it, and then steroids which help fight COVID-19 act like fuel to the fire. In addition, many families have had to treat relatives for COVID-19 at home, meaning people may become exposed to the mold after receiving medicine or oxygen therapy in less-than-sterile conditions.
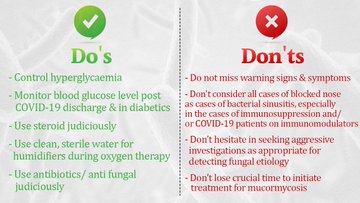
One way to stall the possibility of the fungal infection is to make sure that Covid-19 patients - both in treatment and after recovery - are being administered the right dose and duration of steroids.
Doctors should take care of the sugar levels after the patients are discharged.
They should also consider giving other drugs that control inflammation instead of prescribing steroids.
Above all, maintain a clean and sterile environment around covid patients and also around those who have just recovered from it.
How to prevent Mucormycosis?
1) Use masks if you are visiting dusty construction sites
2) Wear shoes, long trousers, long sleeve shirts and gloves while handling soil (gardening), moss or manure
3) Maintain personal hygiene, including thorough scrub bath
4) The disease can be managed by controlling diabetes, discontinuing immunomodulating drugs, reducing steroids and extensive surgical debridement- to remove all necrotic materials, according to the advisory.
Pics Source: Health ministry, Government of India
If you are in Hyderabad, ENT hospital, Koti, and Gandhi hospital treat this black fungus infection.
PS: People use black, white and yellow fungus to refer to mucormycosis, aspergillosis, candidiasis and cryptococcosis.
For information on white fungus and yellow fungus, please click on this link:
now-we-have-white-fungus-to-deal-with
Qs people asked me on this topic and my replies:
Q: why is black fungus more prevalent in India than in other countries?
Krishna:
Steroids reduce inflammation in the lungs for Covid-19 and appear to help stop some of the damage that can happen when the body's immune system goes into overdrive to fight off coronavirus. But they also reduce immunity and push up blood sugar levels in both diabetics and non-diabetic Covid-19 patients.
It's thought that this drop in immunity could be triggering these cases of mucormycosis.
Diabetes lowers the body's immune defenses, coronavirus exacerbates it, and then steroids which help fight COVID-19 act like fuel to the fire. In addition, many families have had to treat relatives for COVID-19 at home, meaning people may become exposed to the mold after receiving medicine or oxygen therapy in less-than-sterile conditions.
4. Not maintaining clean and sterile environment around covid patients and also around those who have just recovered from it (3).
5. Hot and dusty environments have more fungal spores for people to breathe
Footnotes:
1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6213704/#:~:text=India....
2. https://www.scientificamerican.com/article/why-deadly-black-fungus-...
Views: 299
Replies to This Discussion
-
184
Offlate we have noticed a surge in cases of “MUCORMYCOSIS “ , the black fungus , in “COVID” recovered patients who are diabetic too.
This “black fungus” or “Mucor” is present in dust or soil around us , but generally our immunity is sufficient to repel it efficiently from our bodies.
This “black fungus” or “Mucor” gets access or invades our body once our immunity response is exhausted/ weak/ slow/ inefficient secondary due to conditions like “COVID”, “Diabetes”, “HIV”, “transplant patients on steroids”, and the bodies defenses have lowered the guard due to its inefficiency to act swiftly to kill the fungus.
This fatal disease earlier was considered to be untreatable , atleast before the advent of “Amphotericin B antifungals”.
Cases had 100% mortality rate before 1954.
The dictum is that the disease should be diagnosed fast and treatment started within 6 days, then the chances of survival are high.
Treatment comprises of maintaining the blood sugars in control , “Amphotericin antifungal injection”, and endoscopic evaluation of the paranasal sinuses by a team of “Maxillofacial and ENT surgeons”, maxillectomy of the diseased jaw if needed.
Generally the disease presents as headaches, heaviness around nasal sinus, vomiting in some cases, pain and swelling around eyes , redness in eyes, pain in teeth and jaws, mobility and weakening of teeth, blackish discoloration or alteration of the soft tissue of the oral cavity like a burned “eschar”.
Diagnosis is made by gold standard biopsy histopathology of the tissues harvested and “KOH” mount on slides for staining which gives classical appearance of the fungus as branched aseptate hyphae at right angles.
--
Fungal spores are everywhere, but we are pretty efficient at clearing them from our lungs. “But COVID damages the lung. So then you have a double whammy: reduced capacity to naturally clear the spores and reduced immune response as a result of steroids.”
-
© 2026 Created by Dr. Krishna Kumari Challa.
Powered by
![]()