Science, Art, Litt, Science based Art & Science Communication
What might happen when you take lots of medicines...
One of our uncles died of liver cirrhosis ten years back. He never touched alcohol in his life. He didn't have any viral infection to cause this. He didn't have diabetes, heart problems and he was not obese. Actually there was no reason that doctors could identify that might have caused this condition in him.
But, when they learned that he took lots and lots of medicines even for small ailments like headaches, stomachaches, sleeplessness, they realized reaction to drugs could have caused his condition. He used to take them even as a preventive measure in anticipation of health conditions! Because he was a medical store in-charge of a hospital and he had almost all the medicines at his disposal! I still remember the big blue plastic box in his cupboard he used to keep his medicines in.
My mother used to suffer from several ailments. Diabetes ( sometimes hypoglycemia) , BP, arthritis, osteoporosis, bronchial asthma, oedema, severe anemia, indigestion, sciatica, fungal infection of fingers and toes because of diabetes despite taking several precautions, frequent lung, dental and other infections, weakness because of old age, irregular heart beat, pericardial effusion and in the end brain stroke.
Doctors used to prescribe lots of medicines for her*. One body, multiple drugs: It can be a recipe for disaster! The risk increases with age. And my mother was old and frail! I used to wonder what might happen if she took several medicines for all those conditions mentioned above. I even discussed this with doctors and pleaded with them to prescribe medicines for her only if they're absolutely necessary. I used to ask them to tell me what they were prescribing and why she needed them. And I gave her medicines only that were necessary for her survival.
*When a person 's prescribed several different medications at once in order to treat one or multiple health conditions—the phenomenon is known as polypharmacy. (4)
While giving all those medicines to her ... these things crossed my mind several times...
These are chemicals! Although tested for human safety, clinical researchers usually weigh pros and cons and select the ones whose positives outweigh negatives. But still there will be negatives - what we call side effects. Despite these ill effects we use them because they are necessary for the survival of patients or to prolong their lives. Taking medicines or drugs is a necessary evil in such cases!
And the most important thoughts that disturbed me were ... when people take several medicines like my mother used to ... they can ...
1. Interact with one another
2. produce over dose of a drug because too much of one drug remains in your system because of the interactions
2. reduce or increase the potency of one another if they act in opposite or similar ways
3. nullify one another's potency if one drug can’t be absorbed or metabolized properly
4. produce other toxic and harmful products after reacting with one another inside human bodies
5. interfere with the patient's normal metabolic processes
6. cause damage to body organs
7. cause several other severe health conditions as a result of the above processes
-and this one is a positive one-
8. successfully suppress an existing health condition and help us find a new cure for diseases that don't have medicines yet!
These thoughts of mine have solid base as I know about the research going on in the clinical field ( now I can understand why they say ignorance is a bliss. At least you don't have to worry about these things in the beginning and can have mental peace but only up to a certain extent. When once you and your family members and friends start suffering severely because of your ignorance, the saying sails out through the window . Although we worry a lot because of the knowledge we have, we can take precautions and keep ourselves and our loved ones safe for a long time ).
Interactions can vary from person to person because of changes in the absorption, distribution, metabolism, gut microbes and excretion of the drug within the body. Because of this, drug reactions largely are unpredictable, even with known interactions.
There are hundreds of possible interactions between commonly prescribed medicines that very few people seem to have heard of. People routinely use these medicines, without much thought because, well, they are medicines and are suppose to cure their ailments! Not enhance them. But unfortunately sometimes they do just the second one as a result of drug interactions! So why do they happen, and why do they matter?
The drug interactions happen mostly because of competition!
Some drugs work in complementary or opposite ways at the same sites in the body. If they're given together, they can compete with each other, reducing (or sometimes increasing) the effect of one or both. A good example is the beta-blocker, which is given to people who've had a heart attack or heart failure, or sometimes high blood pressure. If you have asthma, one of the main treatments is an inhaler called a beta agonist (commonly called Ventolin or salbutamol). A beta agonist makes the beta receptors in your body work better - a beta-blocker stops them. If you have asthma, some beta-blockers can bring on an asthma attack or stop your inhaler from working.
Most medicines you take as tablets get into your bloodstream. After a few hours, they're removed through your kidneys or your liver, which act as filters not just for medicines but for all sorts to toxins and products your body makes. Your kidneys and liver are incredibly complicated organs, with hundreds of different chemicals called enzymes working all the time to stop toxins from building up in your body. If two medicines are broken down by the same enzymes, they can interact. That means that, for instance, if you're taking a statin tablet called simvastatin, you shouldn't also take antibiotics like erythromycin or heart tablets called diltiazem, verapamil and amiodarone. Bizarrely, even drinking grapefruit juice can affect how simvastatin is broken down, so taking the two together can lead to dangerously high levels of simvastatin in your system.
Another danger is, if the side effects are similar, they can add up. For example, if you take allopurinol (Lopurin or Zyloprim) for gout and add the drug azathioprine (Imuran) to treat rheumatoid arthritis, the azathioprine can further suppress your immune system, possibly putting you at risk of a serious infection. And, both aspirin and the blood-thinning drug warfarin (Coumadin) decrease your blood's ability to clot, so if you're taking warfarin for cardiovascular disease and aspirin to ease your migraine problem, you could be unknowingly going for a life-threatening bleeding episode!
Sildenafil (viagra) and Nitrate (sorbitrate) tend to cross-react and can create hypotension (BP fall) they are pharmacologically contraindicated as combination.
And - this is very important - many herbal products and medicines from your alternate medicine kits can interact with other medicines. These include 'natural' remedies for depression.
Moreover if you take alcohol or some vitamin and food supplements, they too might interfere with the medicines' potency and sometimes can cause severe toxic effects and even death!
Alcohol often has harmful interactions with prescription medications, over-the-counter drugs, and even some herbal remedies. Alcohol interactions with medications may cause problems such as:
nausea and vomiting, headaches, drowsiness, dizziness, fainting, changes in blood pressure, abnormal behavior, loss of coordination and accidents.
Mixing alcohol and medications also may increase the risk of complications such as:
liver damage, heart problems, internal bleeding, impaired breathing and depression.
In some cases, alcohol interactions may decrease the effectiveness of medications or render them useless. In other cases, alcohol interactions may make drugs harmful or even toxic to the body.
Even in small amounts, alcohol also may intensify medication side effects such as sleepiness, drowsiness, and light-headedness, which may interfere with your concentration and ability to operate machinery or drive a vehicle, and lead to serious or even fatal accidents.
Hundreds of commonly used prescription and over-the-counter drugs may adversely interact with alcohol. These include medications used for: Allergies, colds, and flu, angina and coronary heart disease, anxiety and epilepsy, arthritis, blood clots, cough, depression, diabetes, enlarged prostate, heartburn and indigestion, high blood pressure, high cholesterol, infections, muscle pain, nausea and motion sickness, pain, fever, and inflammation, seizures, severe pain from injury, post-surgical care, oral surgery, migraine and sleep problems.
Alcohol is metabolized in the liver, and a lot of drugs are metabolized via the same pathways. So it has the potential to interact with a whole host of drugs, including things you might not think are related at all.
One should never drink while on antibiotic treatment.
Certain dietary supplements can change absorption, metabolism, or excretion of a medication and therefore affect its potency. You may be getting either too much or too little of a medication you need if you take these supplements. Dietary supplements are widely used by people and include vitamins, minerals, and other less familiar substances—such as herbals, botanicals, amino acids, and enzymes. Children are more vulnerable in case of drug and supplement interactions.
Natural does not always mean safe. For example, many weight loss products claim to be “all-natural” or “herbal,” but their ingredients may interact with medications or may be dangerous for people with certain medical conditions.
My mother used to take several ayurved medicines prescribed by well qualified ayurved doctors for her knee problems. Some 15 years back she developed severe diabetes with her blood sugar levels going up to 500 - 600 mg/dL. The main stream doctors when consulted asked us about the medicines she was taking. When told about the ayurvedic medicines, they asked us to immediately stop using them. They told us some of them contain steroids that enhance the diabetic conditions several fold if people are vulnerable and genetically predisposed to them.
Warfarin (a prescription blood thinner), ginkgo biloba (a herbal supplement), aspirin and vitamin E (a supplement) can each thin the blood. Taking any of these products together may increase the potential for internal bleeding or stroke.
Antibiotics can limit body's ability to uptake analgesics: Disruption of the microbiota, whether induced by dietary changes, antibiotic administration or invasive pathogens, can disturb the balance of the microbiota and alter metabolic networks. These disturbances can affect the biodisposition of certain drugs, which can ultimately lead to adverse drug reactions (2). There are many diverse mechanisms the gut microbiome can use to alter the disposition, efficacy and toxicity of drugs and foreign substances. These can include the expression of enzymes that can activate or inactivate drugs, the direct binding of drugs to a bacterial organism, the reactivation of drugs by microbial expressed enzymes, and the direct competition between the host and microbes for host metabolizing enzymes. For example, an association between pre-dose, gut-derived urinary metabolites and response to the commonly used analgesic acetaminophen has been reported. Research results suggest that exposure to amoxicillin or ampicillin/neomycin can alter the pharmacokinetics and metabolism of acetaminophen, and that these alterations could be due to changes in gut microbiome composition. Shifts in the composition of gut microbiota can disturb the balance of organisms, which can influence the biodisposition of orally administered drugs (3).
Grapefruit juice can be part of a healthful diet—most of the time. It has vitamin C and potassium—substances your body needs to work properly. But it isn’t good for you when it affects the way your medicines work. Grapefruit juice and fresh grapefruit can interfere with the action of some prescription drugs, as well as a few non-prescription drugs. This interaction can be dangerous. With most drugs that interact with grapefruit juice, the juice increases the absorption of the drug into the bloodstream. When there is a higher concentration of a drug, you tend to have more adverse events. For example, if you drink a lot of grapefruit juice while taking certain statin drugs to lower cholesterol, too much of the drug may stay in your body, increasing your risk for liver damage and muscle breakdown that can lead to kidney failure. Drinking grapefruit juice several hours before or several hours after you take your medicine may still be dangerous. So it’s best to avoid or limit consuming grapefruit juice or fresh grapefruit when taking certain drugs. While scientists have known for several decades that grapefruit juice can cause a potentially toxic level of certain drugs in the body, more recent studies have found that the juice has the opposite effect on a few other drugs.
Examples of some types of drugs that grapefruit juice can interact with are:
some statin drugs to lower cholesterol, such as Zocor (simvastatin), Lipitor (atorvastatin) and Pravachol (pravastatin)
some blood pressure-lowering drugs, such as Nifediac and Afeditab (both nifedipine)
some organ transplant rejection drugs, such as Sandimmune and Neoral (both cyclosporine)
some anti-anxiety drugs, such as BuSpar (buspirone)
some anti-arrhythmia drugs, such as Cordarone and Nexterone (both amiodarone)
some antihistamines, such as Allegra (fexofenadine)
Grapefruit juice does not affect all the drugs in the categories above. Ask your health care professional to find out if your specific drug is affected.
The opposite effect grape fruit juice can have on drugs is important too. It involves the transportation of drugs within the body rather than their metabolism, according to doctors. Proteins in the body known as drug transporters help move a drug into cells for absorption. Substances in grapefruit juice block the action of a specific group of transporters. As a result, less of the drug is absorbed and it may be ineffective.
(Don't confuse grape fruit with grapes - some people who read this article have asked me whether they have to stop eating grapes while taking medicines. The grapefruit is a subtropical citrus tree known for its sour to semi-sweet fruit. Grapefruit is a hybrid originating in Barbados as an accidental cross between two introduced species, sweet orange. I am adding pictures of grape fruit and grapes to help you distinguish between the two types of fruits.
Grape fruit
Grapes
So what can you do now after learning about these things? Discuss with doctors! Stick to one doctor, if possible, who knows your complete health profile and the medicines you are taking..
When you're getting a new medicine from your doctors, tell them about all the medicines you're using. Don't fail to recall and let them know about medicine changes from hospital clinics, dentists etc. And don't forget to mention medicines you get without prescription - even paracetamol or aspirin. That way, your healthcare professional can assess the situation properly and reassure you that they're safe to take together.
Many medicines now come with a patient information leaflet, which should tell you about and other medicines yours might interact with.
Adjust the timing. Some medications interfere with others by keeping the second one from being absorbed in the intestine. For example, antacids can interfere with the body's absorption of tetracycline and some other antibiotics. In those cases, just adjusting the timing a bit will alleviate the problem.
Change the dose – or the drug. Sometimes two drugs interact to increase or decrease the effectiveness of the other. Nonsteroidal anti-inflammatory drugs, for example, can blunt the effects of drugs that treat high blood pressure, sometimes making it necessary to increase the dose of the blood pressure medication. If a drug increases the effect of another, lowering the dose of one may help. In other cases, your doctor can switch you to a different drug that provides the benefits without the interaction risk (4).
Monitor closely. In some cases you need all the drugs you are taking, even if they have the potential to interact. When that happens, your doctor will need to monitor you closely, usually through frequent blood tests. Unless a problem is detected, the risk of taking you off a medication – or perhaps even changing the dose – may be worse than the risk of interactions in such situations.
Although this is usually the choice of last resort, doctors must sometimes prescribe a third medication to help alleviate the problems that an interaction between two other drugs is causing! For example, if you need both NSAIDs (non-steroidal anti-inflammatory drugs, also known as NAIDs, non-steroidal anti-inflammatory agents/analgesics) and corticosteroids, yet taking them together causes stomach upset or increases your risk of developing a stomach ulcer, your doctor may prescribe a third drug to ease your stomach upset and reduce your ulcer risk.
The best thing to do is ... please don't take medicines unless they are absolutely necessary and unless your doctor stresses the need to take them. I don't too! And strictly stick to your doctor's advice. Don't tread the path of misadventures by following what your friends, neighbours and relatives suggest if they are not qualified to give you guidance on health issues.
One more thing: gut microbes may contribute to the dramatic variability that is observed in side effects and efficacy between different patients (1). So what we see in labs is not seen inside human bodies making things very complicated.
Watch this video that confirms exactly what I said above:
References:
1. https://medicalxpress.com/news/2019-06-gut-microbes-medication.html...
2. https://medicalxpress.com/news/2020-03-antibiotics-limit-body-abili...
3. Michael A. Malfatti et al. Manipulation of the Gut Microbiome Alters Acetaminophen Biodisposition in Mice, Scientific Reports (2020). DOI: 10.1038/s41598-020-60982-8
4. Leal Rodríguez C, Drug dosage modifications in 24 million in-patient prescriptions covering eight years: A Danish population-wide study of polypharmacy, PLOS Digital Health (2023). DOI: 10.1371/journal.pdig.0000336. journals.plos.org/digitalhealt … journal.pdig.0000336
Latest research on this:
The researchers tested 23 commonly used drugs using this system, allowing them to identify transporters used by each of those drugs. Then, they trained a machine-learning model on that data, as well as data from several drug databases. The model learned to make predictions of which drugs would interact with which transporters, based on similarities between the chemical structures of the drugs.
Using this model, the researchers analyzed a new set of 28 currently used drugs, as well as 1,595 experimental drugs. This screen yielded nearly 2 million predictions of potential drug interactions. Among them was the prediction that doxycycline, an antibiotic, could interact with warfarin, a commonly prescribed blood-thinner. Doxycycline was also predicted to interact with digoxin, which is used to treat heart failure, levetiracetam, an antiseizure medication, and tacrolimus, an immunosuppressant.
To test those predictions, the researchers looked at data from about 50 patients who had been taking one of those three drugs when they were prescribed doxycycline. This data, which came from a patient database at Massachusetts General Hospital and Brigham and Women's Hospital, showed that when doxycycline was given to patients already taking warfarin, the level of warfarin in the patients' bloodstream went up, then went back down again after they stopped taking doxycycline.
That data also confirmed the model's predictions that the absorption of doxycycline is affected by digoxin, levetiracetam, and tacrolimus. Only one of those drugs, tacrolimus, had been previously suspected to interact with doxycycline.
In addition to identifying potential interactions between drugs that are already in use, this approach could also be applied to drugs now in development. Using this technology, drug developers could tune the formulation of new drug molecules to prevent interactions with other drugs or improve their absorbability.
Screening oral drugs for their interactions with the intestinal transportome via porcine tissue explants and machine learning, Nature Biomedical Engineering (2024). DOI: 10.1038/s41551-023-01128-9
----
Study reveals five medication 'prescribing cascades' that may put older adults at risk
"Prescribing cascades" occur when one medication is used to treat or prevent a side effect of another medication. An unintentional cascade can arise when a patient's symptoms are mistaken for a new illness. In that case, the patient not only experiences the original side effect but also faces added risks from the second medication.
Researchers analyzed Irish national prescription data for 533,464 community-dwelling Irish adults aged 65 years and older, covering prescriptions dispensed from 2017 to 2020. The findings are published in The Annals of Family Medicine journal.
A prescription sequence symmetry analysis was performed within a 365-day window to examine nine expert-defined prescribing cascades known as "ThinkCascades." Researchers examined dispensed prescription data only for potential prescribing cascades.
Out of the nine prescribing cascades examined, five had significant positive adjusted sequence ratios, indicating that the patient was more likely to receive the first medication before the second medication:
- Calcium channel blocker leading to diuretic prescribing
- Alpha-1-receptor blocker leading to vestibular sedative prescribing
- Selective serotonin reuptake inhibitor (SSRI) or selective norepinephrine reuptake inhibitor (SNRI) leading to sleep agent prescribing
- Benzodiazepine leading to antipsychotic prescribing
- Antipsychotic leading to anti-Parkinsonian agent prescribing
Three other drug pairs showed significant negative associations, indicating that the patient was less likely to receive the first medication before the second medication:
- Diuretic to overactive bladder medication
- Benzodiazepine to antidementia agent
- Nonsteroidal anti-inflmmatory drugs (NSAIDs) to antihypertensive medication
For clinicians, including adverse drug reactions among the possible causes to confirm or exclude when patients present with new symptoms in primary care is an important step in identifying and mitigating medication-related harm.
Ann Sinéad Doherty et al, Prescribing Cascades Among Older Community-Dwelling Adults: Application of Prescription Sequence Symmetry Analysis to a National Database in Ireland, The Annals of Family Medicine (2025). DOI: 10.1370/afm.240383
Views: 3493
Replies to This Discussion
-
3287
Do Vitamins and Supplements Make Antidepressants More Effective?
Fish oil, Vitamin D and other nutrients appear to raise the potency of medication
http://www.scientificamerican.com/article/do-vitamins-and-supplemen...
--
Don't drink any alcohol if you are taking disulfiram (Antabuse). ... Drinking red winewhile taking felodipine for high blood pressure might cause your blood pressure to go too low. Medications for depression (MAOIs) Interaction Rating: Major Do not take this combination.Wine Effectiveness, Safety, and Drug Interactions on RxList
--Can I take allopathic, homeopathic and Ayurvedic medicines together?Krishna:
-
-
A few medications that may interact with apple cider vinegar:
- Diabetes medication: People who take insulin or insulin-stimulating medications and vinegar may experience dangerously low blood sugar or potassium levels.
- Digoxin (Lanoxin): This medication lowers your blood potassium levels. Taking it in combination with apple cider vinegar could lower potassium too much.
- Certain diuretic drugs: Some diuretic medications cause the body to excrete potassium. To prevent potassium levels from dropping too low, these drugs shouldn’t be consumed with large amounts of vinegar.
- --
Molecular understanding of drug interactions suggests pathway to better malaria treatments
https://medicalxpress.com/news/2020-01-molecular-drug-interactions-...
--
Gut microbes eat your medication ... they may contribute to the dramatic variability that is observed in side effects and efficacy between different patients ...
https://medicalxpress.com/news/2019-06-gut-microbes-medication.html...
--
These Medications Don't Mix Well With Alcohol. An Expert Explains The Risks
A glass or two of champagne with Christmas lunch. A cool crisp beer at the beach. Some cheeky cocktails with friends to see in the New Year. There seem to be so many occasions to unwind with an alcoholic drink this season.
But if you're taking certain medications while drinking alcohol, this can affect your body in a number of ways. Drinking alcohol with some medicines means they may not work so well. With others, you risk a life-threatening overdose.
Here's what you need to know if you're taking medication over Christmas and plan to drink.
Why is this a big deal?
After you take a medicine, it travels to the stomach. From there, your body shuttles it to the liver where the drug is metabolized and broken down before it goes into your bloodstream.
Every medicine you take is provided at a dose that takes into account the amount of metabolism that occurs in the liver.
When you drink alcohol, this is also broken down in the liver, and it can affect how much of the drug is metabolised.
Some medicines are metabolized more, which can mean not enough reaches your bloodstream to be effective.
Some medicines are metabolized less. This means you get a much higher dose than intended, which could lead to an overdose.
The effects of alcohol (such as sleepiness) can act in addition to similar effects of a medicine.
Whether or not you will have an interaction, and what interaction you have, depends on many factors. These include the medicine you are taking, the dose, how much alcohol you drink, your age, genes, sex, and overall health.
Women, older people, and people with liver issues are more likely to have a drug interaction with alcohol.
Which medicines don't mix well with alcohol?
Many medicines interact with alcohol regardless of whether they are prescribed by your doctor or bought over the counter, such as herbal medicines.
1. Medicines + alcohol = drowsiness, coma, death
Drinking alcohol and taking a medicine that depresses the central nervous system to reduce arousal and stimulation can have additive effects. Together, these can make you extra drowsy, slow your breathing and heart rate and, in extreme cases, lead to coma and death. These effects are more likely if you use more than one of this type of medicine.
Medicines to look out for include those for depression, anxiety, schizophrenia, pain (except paracetamol), sleep disturbances (such as insomnia), allergies, and colds and flu.
It's best not to drink alcohol with these medicines, or to keep your alcohol intake to a minimum.
2. Medicines + alcohol = more effects
Mixing alcohol with some medicines increases the effect of those medicines.
One example is with the sleeping tablet zolpidem, which is not to be taken with alcohol. Rare, but serious, side effects are strange behavior while asleep, such as sleep-eating, sleep-driving, or sleep-walking, which are more likely with alcohol.
3. Medicines + craft beer or home brew = high blood pressure
Some types of medicines only interact with some types of alcohol.
Examples include some medicines for depression, such as phenelzine, tranylcypromine, and moclobemide, the antibiotic linezolid, the Parkinson's drug selegiline, and the cancer drug procarbazine.
These so-called monoamine oxidase inhibitors only interact with some types of boutique and artisan beers, beers with visible sediment, Belgian, Korean, European, and African beers, and homemade beers and wine.
These types of alcohol contain high levels of tyramine, a naturally occurring substance usually broken down by your body that doesn't ordinarily cause any harm.
However, monoamine oxidase inhibitors prevent your body from breaking down tyramine. This increases levels in your body and can cause your blood pressure to rise to dangerous levels.
4. Medicines + alcohol = effects even after you stop drinking
Other medicines interact because they affect the way your body breaks down alcohol.
If you drink alcohol while using such medicines you may feel nauseous, vomit, become flushed in the face and neck, feel breathless or dizzy, your heart may beat faster than usual, or your blood pressure may drop.
This can occur even after you stop treatment, then drink alcohol. For example, if you are taking metronidazole you should avoid alcohol both while using the medicine and for at least 24 hours after you stop taking it.
An example of where alcohol changes the amount of the medicine or related substances in the body is acitretin.
This medication is used to treat skin conditions such as severe psoriasis and to prevent skin cancer in people who have had an organ transplant.
When you take acitretin, it changes into another substance – etretinate – before it is removed from your body. Alcohol increases the amount of etretinate in your body.
This is especially important as etretinate can cause birth defects. To prevent this, if you are a woman of childbearing age, you should avoid alcohol while using the medicine and for two months after you stop taking it.
Myths about alcohol and medicines
Alcohol and birth control
One of the most common myths about medicines and alcohol is that you can't drink while using the contraceptive pill.
It is generally safe to use alcohol with the pill as it doesn't directly affect how well birth control works.
But the pill is most effective when taken at the same time each day. If you're drinking heavily, you're more likely to forget to do this the next day.
Alcohol can also make some people nauseous and vomit. If you vomit within three hours of taking the pill, it will not work. This increases your risk of pregnancy.
Contraceptive pills can also affect your response to alcohol as the hormones they contain can change the way your body removes alcohol. This means you can get drunk faster, and stay drunk for longer, than you normally would.
Alcohol and antibiotics
Then there's the myth about not mixing alcohol with any antibiotics. This only applies to metronidazole and linezolid.
Otherwise, it is generally safe to use alcohol with antibiotics, as alcohol does not affect how well they work.
But if you can, it is best to avoid alcohol while taking antibiotics. Antibiotics and alcohol have similar side effects, such as an upset stomach, dizziness, and drowsiness.
Using the two together means you are more likely to have these side effects. Alcohol can also reduce your energy and increase how long it takes for you to recover.
Where can I go for advice?
If you plan on drinking alcohol these holidays and are concerned about any interaction with your medicines, don't just stop taking your medicines.
Your pharmacist can advise you on whether it is safe for you to drink based on the medicines you are taking, and if not, provide advice on alternatives.

Nial Wheate, Associate Professor of the Sydney Pharmacy School, University of Sydney and Jessica Pace, Associate Lecturer, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
https://www.sciencealert.com/these-medications-dont-mix-well-with-a...
-
-
Genetic variants place Asians at higher risk of side effects to common medications
https://medicalxpress.com/news/2020-03-genetic-variants-asians-high...
A few medications that may interact with apple cider vinegar:Diabetes medication: People who take insulin or insulin-stimulating medications and vinegar may experience dangerously low blood sugar or potassium levels.
Digoxin (Lanoxin): This medication lowers your blood potassium levels. Taking it in combination with apple cider vinegar could lower potassium too much.
Certain diuretic drugs: Some diuretic medications cause the body to excrete potassium. To prevent potassium levels from dropping too low, these drugs shouldn’t be consumed with large amounts of vinegar.
--
Molecular understanding of drug interactions suggests pathway to better malaria treatments
https://medicalxpress.com/news/2020-01-molecular-drug-interactions-...--
Gut microbes eat your medication ... they may contribute to the dramatic variability that is observed in side effects and efficacy between different patients ...
https://medicalxpress.com/news/2019-06-gut-microbes-medication.html...
--
Inactive pill ingredients could raise the dose of your medication
Daniel Reker et al. Machine Learning Uncovers Food- and Excipient-Drug Interactions, Cell Reports (2020). DOI: 10.1016/j.celrep.2020.02.094--Ibuprofen and Aspirin especially taken together can cause serious stomach ulcers and stomach bleeds.--Hydroxychloroquine is not effective for treating coronavirus, according to small trial
https://www.quora.com/Do-chloroquine-and-azithromycin-really-work-t...
--
https://medicalxpress.com/news/2020-04-drugs-affect-heart-rhythm.ht...
Computer model predicts how drugs affect heart rhythm
-
-
Combining certain meds with ibuprofen can permanently injure kidneys
Anyone who is taking a diuretic and a renin-angiotensin system (RSA) inhibitor for high blood pressure should be cautious about also taking ibuprofen, according to new research.
Diuretics and RSA inhibitors are commonly prescribed together for people with hypertension and are available under various pharmaceutical brand names. Painkillers such as ibuprofen are available over-the-counter in most pharmacies and stores in popular brands.
Researchers used computer-simulated drug trials to model the interactions of the three drugs and the impact on the kidney. They found that in people with certain medical profiles, the combination can cause acute kidney injury, which in some cases can be permanent.
It's not that everyone who happens to take this combination of drugs is going to have problems. But the research shows it's enough of a problem that you should exercise caution.
Computer-simulated drug trials can quickly produce results that would take much longer in human clinical trials.
The research, in this case, can also speak directly to the many people who are taking drugs for hypertension and may reach for a painkiller with ibuprofen without giving it much thought.
Diuretics are a family of drugs that make the body hold less water. Being dehydrated is a major factor in acute kidney injury, and then the RAS inhibitor and ibuprofen hit the kidney with this triple whammy.
So scientists advice: If you happen to be on these hypertension drugs and need a painkiller, consider acetaminophen instead.
Jessica Leete et al, Determining risk factors for triple whammy acute kidney injury, Mathematical Biosciences (2022). DOI: 10.1016/j.mbs.2022.108809
-
-
Study finds doctors prescribing untested drug combinations with high addiction potential
The Center for Drug Safety and Effectiveness at Johns Hopkins University has led a study into prescription drug use of multiple concurrent central nervous system (CNS)-active drugs. They found widespread combination prescribing of drugs classified as Schedule II controlled substances with a high potential for psychological or physical dependence and with limited combined clinical trial testing.
The paper, "Medical use and combination drug therapy among US adult users of central nervous system stimulants: a cross-sectional analysis," published in BMJ Open, examined patterns of medical amphetamine and methylphenidate stimulant drug use, both substances considered to have a high potential for psychological or physical addiction.
Utilizing prescription drug claims for US adults aged 19 to 64 from a commercial insurance claims database with over 9.1 million continuously enrolled adults, stimulant use was defined as adults filling one or more stimulant prescriptions in a single year.
The study identified 276,223 individuals (3.0%) using Schedule II stimulants in 2020. They filled a median of eight prescriptions that provided 227 days of exposure. Among this group, 125,781 (45.5%) combined use of one or more additional CNS active drugs for a median of 213 days. Also, 66,996 (24.3%) stimulant users used two or more additional CNS-active medications for a median of 182 days. Among stimulants users, 131,485 (47.6%) used an antidepressant, 85,166 (30.8%) filled prescriptions for anxiety/sedative/hypnotic medications and 54,035 (19.6%) received opioid prescriptions.
Many adults using Schedule II stimulants simultaneously use one or more additional CNS-active drugs. As these can have tolerance and withdrawal effects or potential recreational abuse, the authors suggest that "discontinuation may be challenging," which is another way of stating that these individuals have likely formed a habitual dependence or addiction possibly requiring intervention or rehabilitation.
Once treatment has started, 75% of patients become long-term users. This underscores the possible risks of non-medical guideline use, noting the issues that warranted the classification of these drugs as having a high potential for psychological or physical dependence and their prominent appearance in toxicology drug rankings of fatal overdose cases.
Thomas J Moore et al, Medical use and combination drug therapy among US adult users of central nervous system stimulants: a cross-sectional analysis, BMJ Open (2023). DOI: 10.1136/bmjopen-2022-069668
-
-
How to take vitamins:
Water-Soluble Vitamins: Water-soluble vitamins, such as vitamin C and the B vitamins (including thiamine, riboflavin, niacin, vitamin B6, vitamin B12, biotin, pantothenic acid, and folate), are generally better absorbed when taken with food. This is because the presence of food in the stomach slows down the digestion process, allowing more time for these vitamins to be absorbed. Taking these vitamins with a meal that contains some fat can also enhance their absorption, as they are often soluble in fat.
Fat-Soluble Vitamins: On the other hand, fat-soluble vitamins, such as vitamins A, D, E, and K, are best absorbed when taken with a meal that contains some dietary fat. Fat-soluble vitamins are absorbed along with dietary fats in the small intestine. Therefore, taking them with a meal that contains fat aids in their absorption and utilization by the body.
Iron and Calcium: Certain minerals, such as iron and calcium, also have specific recommendations regarding their timing of intake. Iron supplements are generally recommended to be taken on an empty stomach, as they are better absorbed in an acidic environment. However, if iron causes gastrointestinal discomfort, it can be taken with a small amount of food. Calcium, on the other hand, is better absorbed when taken with food, as it requires stomach acid for optimal absorption.
Medication Interactions: It is important to note that certain medications may interact with vitamins and minerals, affecting their absorption or efficacy. For example, certain antibiotics, antacids, and medications used for thyroid disorders can interfere with the absorption of specific vitamins or minerals. Therefore, if you are taking any medications, it is advisable to consult with your healthcare provider or pharmacist to determine the best time for your vitamin intake.
In summary, the optimal timing for vitamin intake depends on the type of vitamin and whether it is water-soluble or fat-soluble. Water-soluble vitamins are generally better absorbed when taken with a meal, while fat-soluble vitamins are best absorbed when taken with a meal that contains some dietary fat. It is also important to consider any medication interactions that may affect the absorption of vitamins and minerals.
-
-
**
Extreme heat and some medicines can be a risky combo. Here's what to know
https://medicalxpress.com/news/2024-07-extreme-medicines-risky-comb...
-
-
Grapefruit Juice Can Kill You, Evidence Shows
Humans are soft squishy bags of blood that are fairly resilient in many ways, but there are a lot of hazards out there that can cause serious problems, if we're not careful.
And they don't always announce themselves, either. Sometimes the most benign appearance can hide potential dangers. Take the grapefruit juice you might be enjoying with your morning meal. For most people, it's delicious, reasonably healthy, and full of vitamins and minerals.
Mix it with the wrong medication, though, and grapefruit is potentially fatal.
A growing body of research has shown two members of a class of chemical compounds called furanocoumarins that are found in high concentrations in grapefruit can reduce or enhance the uptake of certain drugs. This results in dangerously low – or, as is more often the case, dangerously high – levels of those drugs in the system.
The two drug-interacting furanocoumarins are not just in grapefruits, either. The compound bergamottin can also be found in pomelos and bergamot oranges, and dihydroxybergamottin in pomelos and Seville oranges, the latter of which is often used to make marmalade. (Grapefruits are the result of a pomelo-orange hybrid.)
As pharmacologist Shiew Mei Huang of the FDA explained, "the juice lets more of the drug enter the blood… When there is too much drug in the blood, you may have more side effects."
Here's how it works. Your body produces an enzyme called Cytochrome P450 3A4 (or CYP3A4), mainly in the liver and small intestine. This enzyme helps your body break down small foreign molecules, such as toxins or drugs, so that you can flush them out. It plays a crucial role in the metabolization of many drugs.
 Grapefruit juice can block the action of enzymes that break down some medications.
Grapefruit juice can block the action of enzymes that break down some medications. Furanocoumarins interfere with your body's ability to produce or effecetively use CYP3A4 (and other members of the cytochrome P450 enzyme family). Just a single glass of grapefruit juice can interfere with CYP3A4, and repeated consumption reduces CYP3A4 liver activity.
This, in turn, interferes with your body's ability to metabolize certain oral drugs. More of the drug enters your blood, and it stays in your body for longer, producing an overdose effect even when you have taken the right dosage. And the types of drugs implicated are wide-ranging, from cholesterol and blood pressure medication, to cancer drugs, to anti-anxiety medication.
The results of this can be pretty dramatic. Rapid heartbeat, breakdown of muscle tissue, bone marrow toxicity, shortness of breath, gastrointestinal bleeding, and kidney failure are all complications of some of the medications that are affected by furanocoumarins.
And, in extreme but also seemingly rare cases, these interactions can be fatal.
With some medications, grapefruit can have the opposite effect. With fexofenadine, for example – an antihistamine – consumption of grapefruit reduces the efficacy of the medication. Although the potential side effects aren't as severe, it's certainly not ideal to suddenly find your allergy medication not as effective as you need it to be.
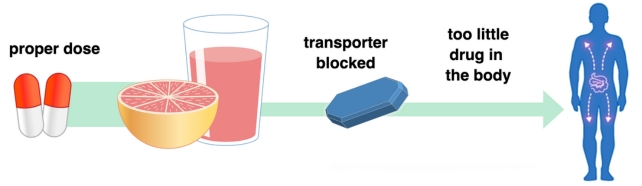
Grapefruit juice can block transporters that carry some medications into the body's cells. (FDA /Michael J. Ermarth/ CC BY-SA 4.0/Wikimedia Commons)
If you're taking important medication, you don't necessarily need to avoid grapefruit like you're a vampire and grapefruit is holy water. But do ask your doctor or pharmacist if you need to be aware of any potential interactions, and make sure you read any information provided with your medication.
And maybe just reach for a glass of water to wash it down
https://www.tandfonline.com/doi/abs/10.1300/J088v08n03_05
https://www.sciencealert.com/grapefruit-juice-can-kill-you-evidence...
-
-
Dosage tweaks may hint at undiscovered interactions between medications
Analysis of data from more than 1 million Danish inpatients identifies nearly 4,000 drug pairings that are associated with more frequent dosage adjustments when prescribed together—potentially hinting at previously undiscovered drug interactions. Scientists presented these findings in the open-access journal PLOS Digital Health.
In some cases, especially among elderly populations, a person may be prescribed several different medications at once in order to treat one or multiple health conditions—a phenomenon known as polypharmacy. Polypharmacy is associated with increased health risks due to the potential for harmful interactions between different drugs. Polypharmacy research has typically focused on the number and type of drugs a patient receives. However, the dosage of each drug may also influence interactions and health outcomes.
To deepen understanding of polypharmacy in the context of drug dosage, researchers analyzed data from the electronic health records of more than 1 million patients admitted as inpatients in Danish hospitals from 2008 to 2016. They used a statistical approach known as Bayesian inference to identify drug pairings associated with more frequent adjustments to the dosage of the drugs.
Out of 77,249 total drug pairings, 3,993 were associated with more frequent dosage adjustments when given together. Further analysis showed that, of the pairs associated with more frequent dosage adjustments, 2,412 were also associated with hospital readmission, mortality, or longer hospital stays, and 308 were associated with worsened kidney function.
Many of the drug pairs associated with dosage adjustments have already been linked by previous research to potential harmful drug interactions.
However, 694 have not, and while this study does not prove any cause-effect relationships, the authors suggest that some of these drug pairings may involve previously undiscovered interactions. These are often given to fewer patients and therefore harder to detect in small scale studies—contrary to the 185 million treatment episodes used in this study. Future research will be needed to explore that possibility.
Overall, these findings help deepen understanding of links between drug dosage and polypharmacy, and could help guide future evaluation of drug interactions and efforts to reduce the risks of polypharmacy for patients.
Leal Rodríguez C, Drug dosage modifications in 24 million in-patient prescriptions covering eight years: A Danish population-wide study of polypharmacy, PLOS Digital Health (2023). DOI: 10.1371/journal.pdig.0000336. journals.plos.org/digitalhealt … journal.pdig.0000336
-----
The most common risk associated with vitamin B12 is an overdose. Too much of this nutrient can cause adverse effects like nausea, vomiting, and diarrhea, and even serious health issues such as liver or kidney damage. Vitamin B12 is also unable to be adequately absorbed without certain acids found in the stomach or intestine, which can make the consequences of an overdose even more serious.
Another risk associated with vitamin B12 is the potential for interactions with other medications. While vitamin B12 is generally considered safe, it can react negatively with certain medications, such as certain antibiotics and chemotherapy drugs. Thus, it’s important to speak to your doctor before combining vitamin B12 and any other medications.
It’s also important to note that some people have a greater risk of developing a vitamin B12 deficiency or experiencing an adverse reaction from taking a large dose of this nutrient. People with certain health conditions, such as pernicious anemia, may have difficulty fully absorbing vitamin B12 from food, so they may be more likely to experience an overdose.
In addition, vegans and vegetarians are at an increased risk for developing a vitamin B12 deficiency, and thus, might require supplementation of this nutrient. However, due to the risks associated with vitamin B12, it is important that these individuals speak to their doctor about the appropriate dosage and timing of supplementation.
Overall, it’s important to recognize that vitamin B12 is an essential nutrient, but it’s also important to be aware of the potential risks associated with taking too much of it. Speak to your doctor for guidance on how to best incorporate this nutrient into your diet or use supplementation if necessary.
---
Vitamin B12 is actually not dangerous when taken in appropriate doses. In fact, it is an essential vitamin that is necessary for many bodily functions, including the production of red blood cells and the maintenance of a healthy nervous system.
However, excessive doses of vitamin B12 can be harmful. This is because the body has a limited ability to absorb and use vitamin B12, and excess amounts can accumulate in the body and lead to toxic effects.
Additionally, certain medical conditions or medications can interfere with the body's ability to absorb vitamin B12, leading to deficiencies. This can cause a range of health problems, including anemia, fatigue, weakness, and neurological symptoms.
Overall, it's important to get an appropriate amount of vitamin B12 in your diet or through supplements, but excessive doses should be avoided. If you have any concerns about your vitamin B12 levels, it's always a good idea to consult with a healthcare professional for guidance.
-
-
What Drinking While on Medication Can Do to Your Body
Anyone who has drunk alcohol will be familiar with how easily it can lower your social inhibitions and let you do things you wouldn't normally do.
But you may not be aware that mixing certain medicines with alcohol can increase the effects and put you at risk.
When you mix alcohol with medicines, whether prescription or over-the-counter, the medicines can increase the effects of the alcohol or the alcohol can increase the side-effects of the drug. Sometimes it can also result in all new side-effects.
How alcohol and medicines interact
The chemicals in your brain maintain a delicate balance between excitation and inhibition. Too much excitation can lead to convulsions. Too much inhibition and you will experience effects like sedation and depression.
Alcohol works by increasing the amount of inhibition in the brain. You might recognise this as a sense of relaxation and a lowering of social inhibitions when you've had a couple of alcoholic drinks.
With even more alcohol, you will notice you can't coordinate your muscles as well, you might slur your speech, become dizzy, forget things that have happened, and even fall asleep.
Medications can interact with alcohol to produce different or increased effects. Alcohol can interfere with the way a medicine works in the body, or it can interfere with the way a medicine is absorbed from the stomach. If your medicine has similar side-effects as being drunk, those effects can be compounded.
Not all the side-effects need to be alcohol-like. Mixing alcohol with the ADHD medicine ritalin, for example, can increase the drug's effect on the heart, increasing your heart rate and the risk of a heart attack.
Combining alcohol with ibuprofen can lead to a higher risk of stomach upsets and stomach bleeds.
Alcohol can increase the break-down of certain medicines, such as opioids, cannabis, seizures, and even ritalin. This can make the medicine less effective. Alcohol can also alter the pathway of how a medicine is broken down, potentially creating toxic chemicals that can cause serious liver complications. This is a particular problem with paracetamol.
At its worst, the consequences of mixing alcohol and medicines can be fatal. Combining a medicine that acts on the brain with alcohol may make driving a car or operating heavy machinery difficult and lead to a serious accident.
Who is at most risk?
The effects of mixing alcohol and medicine are not the same for everyone. Those most at risk of an interaction are older people, women and people with a smaller body size.
Older people do not break down medicines as quickly as younger people, and are often on more than one medication.
Older people also are more sensitive to the effects of medications acting on the brain and will experience more side-effects, such as dizziness and falls.
Women and people with smaller body size tend to have a higher blood alcohol concentration when they consume the same amount of alcohol as someone larger. This is because there is less water in their bodies that can mix with the alcohol.
What drugs can't you mix with alcohol?
You'll know if you can't take alcohol because there will be a prominent warning on the box. Your pharmacist should also counsel you on your medicine when you pick up your script.
The most common alcohol-interacting prescription medicines are benzodiazepines (for anxiety, insomnia, or seizures), opioids for pain, antidepressants, antipsychotics, and some antibiotics, like metronidazole and tinidazole.
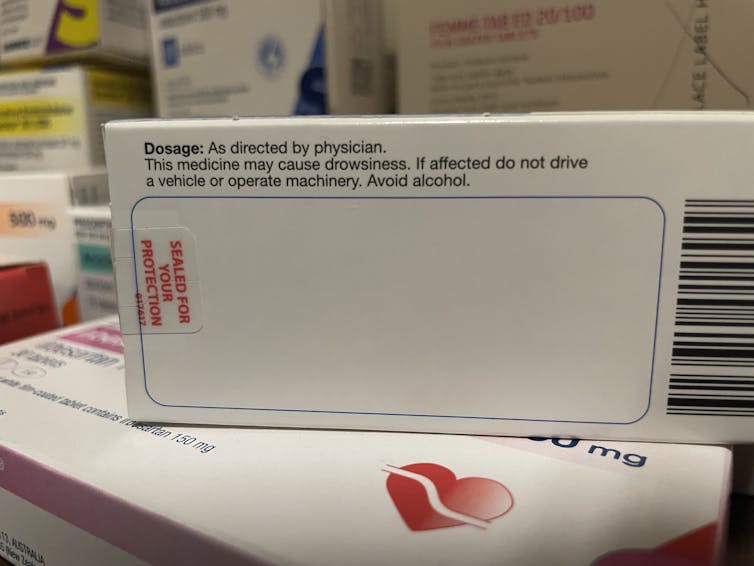
Medicines will carry a warning if you shouldn't take them with alcohol. (Nial Wheate)It's not just prescription medicines that shouldn't be mixed with alcohol. Some over-the-counter medicines that you shouldn't combine with alcohol include medicines for sleeping, travel sickness, cold and flu, allergy, and pain.
Next time you pick up a medicine from your pharmacist or buy one from the local supermarket, check the packaging and ask for advice about whether you can consume alcohol while taking it.
If you do want to drink alcohol while being on medication, discuss it with your doctor or pharmacist first.

Nial Wheate, Associate Professor of the School of Pharmacy, University of Sydney; Jasmine Lee, Pharmacist and PhD Candidate, University of Sydney; Kellie Charles, Associate Professor in Pharmacology, University of Sydney, and Tina Hinton, Associate Professor of Pharmacology, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
-
-
Here's what supplements you really shouldn't take together
While some pills are designed to improve your health, some taken together can cause more harm than good.
Sometimes, our body needs a helping hand. While the well-oiled machine should run perfectly well with a balanced diet and exercise, a bit of metaphorical lubricant can keep you performing at the highest level.
This is where supplements come in. A vast array of vitamins, herbs and plants with purported health benefits are available to us. But not all of these remedies agree with each other.
Take calcium carbonate, for example. This is taken in the form of a tablet to treat symptoms caused by too much stomach acid. It’s a pretty common treatment, used to manage heartburn, indigestion, an upset stomach or more serious acidity issues.
However, for some, this commonly taken medicine has an enemy. “High doses of some minerals may interfere with absorption of other minerals through a variety of mechanisms. Calcium carbonate tends to cause problems for iron supplements.
To be best absorbed, iron supplements need a comfy bed of stomach acid to settle into. This puts it in direct opposition to antacids containing calcium carbonate.
This is just one of the many examples where supplements act against each other, reducing their effects or outright removing the benefits altogether.
-
-
Grapefruit Can Mess With Your Meds, But Scientists May Have a Solution
We know grapefruit has numerous health benefits, but its ingredients can also mess with regular meds, enhancing them to dangerous levels or weakening them so they're no longer effective – a problem that new research might have a solution for.
It's primarily the compounds called furanocoumarins inside grapefruit that interfere with prescription drugs (more than 100 of them, at the last count), which is why people on these meds are often advised to cut out certain fruits from their diet.
But what if that wasn't a concern?
A team from The Volcani Center in Israel decided to look for the genes behind furanocoumarins in the citrus fruits, grapefruit and pomelo. They were able to find a multi-gene cluster in the 2-oxoglutarate-dependent dioxygenase (2OGD) family that was responsible for producing the defensive plant compounds.
Knowing this information opens up the possibility of genetically engineering grapefruits and pomelos without furanocoumarins. Other citrus fruits, including oranges and mandarins, do not naturally produce these compounds.
"This research helps us to understand why fruit of certain citrus species produce furanocoumarins and demonstrates how breeders and researchers could develop furanocoumarin-free citrus varieties," says plant scientist Yoram Eyal, from The Volcani Center.
The study team used a combination of techniques to identify the 2OGD cluster, including DNA and RNA analysis, gene comparisons, and cross-breeding between fruits to highlight variations in furanocoumarin production.
Different genes in the 2OGD cluster were shown to be responsible for its production in different parts of the plant (such as the leaves and the roots), or under different conditions (such as when tissues are under attack). The integrity of one gene in particular, Cg2g000710, seems to be crucial in cooking up furanocoumarins.
What's more, a specific sequence of DNA called the 655-base insertion sequence seems to be disrupting the activity of the Cg2g000710 gene in citrus fruits without furanocoumarins. This may be due to the evolution of these plants over time, the researchers suggest.
"Analysis of genomic and transcriptome sequences of Cg2g000710 and its orthologues demonstrated an intact reading frame in the 'Hudson' grapefruit leaf transcriptome and in the pomelo genome," write the researchers. "In stark contrast, the transcript was entirely absent from the 'Ora' mandarin transcriptome… "
This is some high-level biology, but the key takeaway is that furanocoumarin production has been mapped in citrus fruits for the first time. The researchers didn't attempt to produce furanocoumarin-free grapefruit, but we now have the knowledge and tools that make it possible.
That could help prevent some pretty severe consequences of fruit-drug interactions. Further research will be needed to investigate how these altered citrus fruits could be made – without drastically affecting their taste or introducing other harmful effects.
"Our work provides the basis for future marker-assisted or genome-editing-based breeding of citrus varieties which will be safe for consumption by a large and growing population of humans dependent on the use of prescription drugs," write the researchers.https://nph.onlinelibrary.wiley.com/doi/epdf/10.1111/nph.20322
-
© 2026 Created by Dr. Krishna Kumari Challa.
Powered by
![]()